Hi POCUS pros,
Congrats to Les Bleus on a sweet World Cup win and on the soccer world for teaching us how to feign catastrophic illness severity (some of those collisions looked like they had an Injury Severity Score of at least 76). But enough of that, let’s get your week kicked off right with a healthy dose of cool POCUS cases from the last week.
The Case
Our first case comes from patient LB Munchausen. The patient is in pretty bad shock with a blown RV:

Whilst scanning for the IVC, you see this that makes you feel very bleu for the patient indeed:

Zut alors! Qu’est-ce qui se passe? Ça a l’air colon comme situation!
Case of the Geek
Our second case comes from a patient admitted with severe liver failure. He becomes transiently bradycardic and pre-arrests so a temporary pacer is inserted. Unfortunately, on the confirmatory X-ray we aren’t quite sure where it wound up. So we turn to POCUS

What the…?
Zut alors again! Right?
Answer to Last Weeks Case
The good/the stomach: The image from the top shows a normal appearing stomach with rugae and even a feeding tube in situ for good measure (screen right). The stomach is a common source of false positives given it’s somewhat strange appearance, especially when it coursing near the diaphragm or just below the spleen in the left upper quadrant. Avoid intervening on this normal friend or your patient will never make it to the hotdog eating contest.
The bad/the liver: Again from the top image but screen left. That does look like liver, but why is it all the way over in the left costophrenic angle? Can’t be the spleen, the patient just had a splenectomy for myelofibrosis remember. Myelofibrosis can result in significant hepatomegaly from extra medullary hematopoiesis which is why this patient’s liver is so HUUUUGE (thanks Donald).
The ugly/the abscess: The bottom image shows a round/cyst like structure in the posterior left upper quadrant right where the spleen usually is. If you look closely, you’ll notice debris around the wall especially near the bottom (remember the hematocrit sign?). That post-op abscess is the likely source of her Staph aureus bacteremia and is filled with more golden coccus than the letters on Trump tower.
Answer to Last Weeks Case of the Geek
So this is a tough case. We clearly see a lady with a dilated cardiomyopathy, low EF and severe MR hitting the back wall of the left atrium. Slam-dunk cardiogenic shock right? Remember why the LV dilates though, the EF goes down but the dilation makes the stroke volume stay ok in a lot of patients (at least at rest). That’s why many of these patients are out and about living their regular beta-blocked lives in the community.
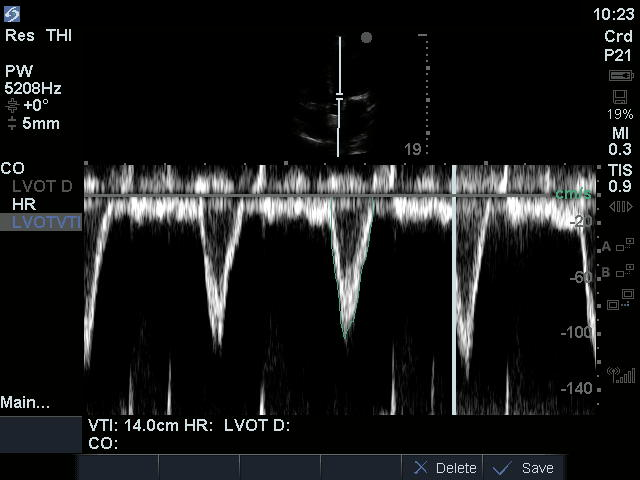
With LVOT D of 2cm, LVOT r is 1cm, the LVOT area is estimated with pi x rsquared so pi x 1squared so pi
SV is LVOT area x LVOT VTI (think of it as a cylinder) so pi x 14 here so: 44
CO is SV x HR so 44 x 110 : 4,4L/min
4.4L/min is decent right?
Well in day to day relaxed life it is, not when you add distributive shock on top of it, which is what happened to this lady with likely necrotizing pneumonia. The heart can’t adapt to the increased workload of distributive shock (which decreases resistance and so necessitates increased CO to maintain MAP). You can try to increase CO (with inotropes) but the main problem here is distributive shock. This type of situations serves to illustrate how an already compromised heart can be ok at steady-state but can’t adapt to an added stressor (often septic shock) and why the LVOT VTI and CO estimations can help you see the true physiological problem the patient is suffering from. I hope your CuriOsity is quenched (see what I did there!). For great cases like these, be sure to check out the hemodynamic series at westernsono.ca
The post Case of the Week: July 23, 2018 appeared first on Western Sono.